One of the biggest challenges faced by medical staff treating COVID-19 is the fact that among newly admitted patients, they do not know who will become a symptomatic patient who requires intensive treatment such as respiratory tube insertion or kidney dialysis.
In general, young people rather than older people often pass lightly even if they get Corona 19, and those with underlying diseases such as heart disease, high blood pressure, and diabetes are known to be more at risk. The problem, however, is that not everyone does. This is because many of the younger under 40 years of age or confirmed patients with no underlying disease have become severely ill.

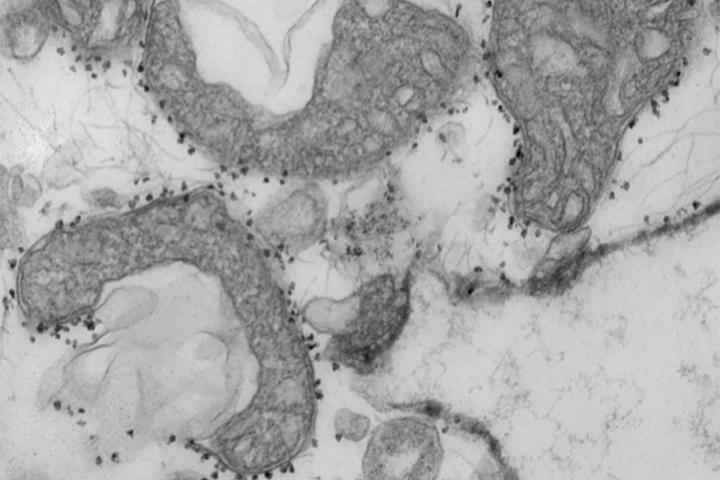
A simple and fast blood test method has been developed that can predict whether COVID-19 patients are at high risk of serious complications or death. The photo shows the damaged mitochondria (dark gray area) released from human lungs. ⒸWANDY BEATTY
Because some patients know they will get better without intensive care, doctors want to know how to assess a patient’s condition as soon as possible.
In this situation, a simple and fast blood test method has been developed that can predict which corona19 patients will have a high risk of serious complications or death within one day of hospitalization. The test, developed by scientists at the University of Washington School of Medicine, was published in the journal JCI Insight in the American Academy of Clinical Research (ASCI) on January 14th.
Higher numbers are twice as likely to die
The researchers measured mitochondrial DNA levels in 97 new patients admitted to the University of Washington University Hospital in Barnes. The level of mitochondrial DNA, a unique type of DNA molecule that usually exists inside a cell’s energy plant, can be measured with a blood test.
The leakage of mitochondrial DNA from cells into the bloodstream is a sign that certain types of cell death are taking place in the body. The researchers found that mitochondrial DNA levels were much higher in patients who died or were admitted to respiratory tract or intensive care units. The researchers also found that the association had nothing to do with the patient’s age, sex, or underlying disease.
Studies have shown that mitochondrial DNA levels are about 10 times higher in patients who develop severe lung dysfunction or eventually die. In addition, patients with higher numbers were found to have a 6 times greater probability of inserting a respiratory tube, 3 times more likely to enter the intensive care unit, and 2 times more likely to die than those who do not.
Dr. Andrew Gelman, who participated in the study, said, “We still don’t understand too much about this disease. Our study shows that mitochondrial DNA flowing into the bloodstream is an inflammatory molecule, so it is itself a factor in tissue damage.” It suggests that it could be the cause.”
The researchers argued that the test could not only be used as a tool to predict disease severity and to better design clinical trials, but it could also identify patients who might benefit from a particular study treatment.
They also said they wanted to evaluate whether the test could be a way to determine the effectiveness of the new treatment. Because effective treatments can lower mitochondrial DNA levels.
Results come out within 1 hour using existing PCR equipment
Professor Hrishikesh Kulkarni, co-author, said, “A larger experiment will be needed to confirm what we have found, but if the patient’s blood pressure is not too low during the first 24 hours of “If you can determine whether you need a respiratory tract or medication, you can change the way patients are classified and manage them more efficiently.”
It is known that the new blood test method developed by the researchers can predict not only the existing indications of inflammation measured in patients hospitalized with Corona 19, but also results beyond. According to the researchers, most other indications of inflammation measured in COVID-19 patients, including those still under investigation, are general indications of systemic inflammation rather than specific inflammation associated with apoptosis.
“Virus can cause tissue damage called necrosis, which is an inflammatory response to infection,” said Dr. Andrew Gelman.
“As the cell opens, its contents, including mitochondrial DNA, are released, which in itself causes inflammation.” There was evidence of damage to these types of cells and tissues in the lungs, heart, and kidneys in patients with Corona 19.
The researchers claim that this test method can be performed quickly and conveniently in most hospital environments, as it uses the same equipment as the machine that handles standard PCR tests for COVID-19. The test, which can quantify mitochondrial DNA levels directly from the blood, does not require an intermediate step to extract DNA, so the results are known to be available within an hour.
The researchers said they want the blood testing method they developed to be validated in a larger central research center before filing for approval with the US Food and Drug Administration (FDA).
(852)